


In 2023, the US shockingly spent 17.6% of its GDP only on health, and since then, healthcare costs have been climbing rapidly. The reason? Aging population, increasing chronic patients, and operational efficiency in clinics of all sizes.
The ones that are most affected and under pressure are the CFO’s, who have to maintain profitability while delivering high-quality care. And with traditional cost-cutting methods like labour reductions or supply chain tweaks, which are not working efficiently anymore, the burden is only increasing.
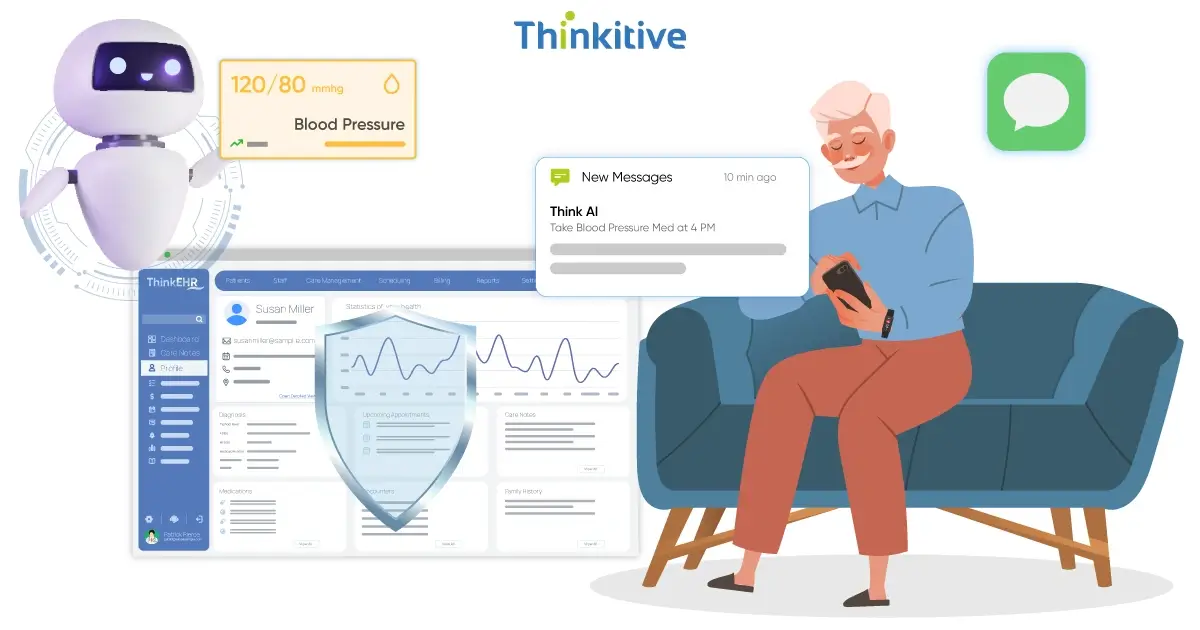
This is where AI-driven cost-cutting solutions are making everything easy for the finance people in healthcare.
With tools that can automate billing and optimize revenue cycles while telling where to allocate resources, healthcare clinics reduce waste and improve efficiency. But this only happens if you know where to invest and what tools to use.
If not, then instead of simplifying, everything can get more complex and take a bad situation from bad to worse.
That’s why we have created this guide that will walk you through the whole process of understanding AI cost savings in healthcare and choosing the AI RCM savings tools that can really help.
Let’s get started!
Financial professionals face the nightmare of balancing high-quality care with increasing healthcare costs. However, while doing so, they are facing many hurdles, one of those being rising operational costs.
With skyrocketing labour costs, constant tech upgrades, and an ever-changing regulatory landscape, maintaining a proper budget is hard. And with stagnated reimbursement rates, recovering or staying profitable is not easy.
Whether it’s Medicare, Medicaid, or a private insurer, the payments are often delayed, and many healthcare providers are underpaid. Also, the reimbursement rates have stagnated for a long time, and with no guarantee of increasing, covering all the costs is challenging.
To add to this already raging inferno, patients' expectations of value-based care and increased competition in the market are driving the pressure high. And because of all this, strategic cost management has become compulsory.
Clinics are in need of smarter ways to save money, better allocate resources, and streamline workflows without compromising patient care.
When a healthcare CFO adopts AI in clinical operations, it is not just a tech decision; it’s a strategic one, too. This is why, without a solid business case, even the most promising AI tool can become a dead investment.
Here, AI budget planning needs to start with a clear cost-benefit analysis framework. CFOs should weigh each potential investment against its projected impact on cost savings, labor efficiency, revenue improvement, and long-term scalability.
An effective healthcare AI investment strategy involves realistic implementation timelines and phased rollouts. Jumping into a full-scale deployment without understanding integration demands or clinical workflows can derail both budgets and expectations. Mapping out each deployment phase, along with its associated costs and staffing needs, helps prevent budget overruns and disruption.
But planning doesn’t stop there. Any AI initiative comes with financial risks, whether from vendor lock-in, regulatory non-compliance, or tech underperformance. That’s where risk assessment and mitigation come into play. CFOs should proactively identify financial exposure points and develop fallback plans, from pilot testing to vendor SLAs and data security safeguards.
To ensure your AI investments actually deliver value, you need a robust performance measurement framework. Define key performance indicators (KPIs) tied to financial outcomes, like reduced claim denials, improved collections, or operational throughput. These metrics not only prove ROI but also guide ongoing optimization.
AI won’t fix your margins overnight. However, disciplined planning and financial accountability become powerful levers for driving sustainable cost control and value-based growth.
Behind every patient encounter lies a mountain of back-office tasks that drain time, money, and staff resources. For CFOs looking to improve margins without cutting corners, AI back-office automation offers a compelling path forward. From front-desk workflows to HR operations, AI is proving its value in reducing administrative overhead while boosting healthcare operational efficiency.
Let’s start with appointment scheduling and management. AI-powered tools can auto-fill calendars, detect gaps, and optimize provider availability in real-time. By reducing appointment overlaps, bottlenecks, and no-shows, these systems not only save administrative labor but also improve patient flow and revenue predictability.
Next comes patient communication automation. Chatbots and automated messaging platforms can handle a wide range of routine tasks—from confirming appointments and sending reminders to answering FAQs and sharing post-visit instructions. The result? Lower call volumes, faster response times, and less reliance on overstaffed support teams.
On the payer side, insurance verification and prior authorization, once time-consuming manual tasks, are now being handled by AI in seconds. These systems pull real-time eligibility data, flag missing information, and even pre-fill forms to reduce friction and speed up care delivery.
Even HR and payroll operations aren’t off-limits. AI tools now assist with scheduling optimization, payroll accuracy checks, credentialing workflows, and even predictive staffing to align labor needs with clinic demand.
In short, when you automate overhead, you free up both capital and human bandwidth. And in today’s margin-squeezed environment, that’s not just an efficiency gain, it’s a strategic advantage.
An inefficient revenue cycle is like a wound that slowly bleeds revenue from a healthcare organization. With each delayed claim, denied reimbursement, and coding error, the loss of revenue increases and stacks up. That’s why more CFOs are turning to healthcare financial AI and using the right RCM saving tools.
First, these tools take out the traditional claim processing procedures and bring in the AI-powered processes. This makes the whole process automated, eliminating manual entries and the errors that come with them. Claims are generated, validated, and then submitted as per the regulatory guidelines without any human intervention. The result? Fewer rejections, faster processing, and healthier cash flow.
Then it solves the biggest problem, denial management. AI analyzes the patterns in claim denials and works to fix them. For instance, codes are not being filed right with every two reports, so it will recheck the codes before submitting the claim. It also learns over time and prevents future denials by validating and proactively correcting mistakes.
Most importantly, AI knows how to code correctly. AI tools can review clinical documentation and suggest compliance with CPT, ICD-10, and HCPCS codes, minimizing the risk of filing incorrect codes. This saves the clinic the trouble of going through audits for frequent coding errors while maximizing reimbursements.
Finally, the process that all finance guys work on for payment posting and reconciliation can be automated. So, recording the payments and then verifying them becomes much faster and accurate, without missing a single payment.
Operations are what run any care smoothly, but if done inefficiently, they can be the reason for significant revenue loss. From redundant workflows to provider burnout, everything needs to be done smoothly, or it can quickly inflate expenses. However, now with operations optimization AI, the picture is changing.
It automates all the manual and repetitive tasks that eat up providers' time and energy. Documentation process can be automated with tools like AI-powered ambient scribe assistants, and reduce charting time significantly with its generative note summarization. This not only reduces burnout but also increases time allocated to patient care.
After this comes workflow optimization. In clinical care, workflows are like the nervous system that keeps the body active. But often, it gets blocked with various challenges, and AI systems identify these bottlenecks and work to solve them. They can suggest and automate changes that improve throughput, reduce wait times, and eliminate duplication, leading to better clinical efficiency.
One thing that troubles administrators is how to optimize resource allocation, so it does not go to waste, and AI tools solve this problem. AI algorithms forecast patient volumes, need for beds, and optimize provider schedules accordingly. Plus, it can tell how much diagnostic equipment you are going to need. The result is leaner operations, smarter staffing, and less capital expenditure on underutilized resources.
Lastly, quality improvement and risk reduction are much easier with AI. With predictive tools, clinics know which patients need help urgently. This leads to on-time interventions and prevention of avoidable complications. This improves outcomes along with protecting clinics from costly readmissions and malpractice claims.
In short, cost containment AI isn’t just about saving costs, but also about delivering better care, more efficiently.
Today, with increasing healthcare costs and patient expectations, CFOs are under huge pressure to reduce costs while maintaining high-quality care. But the good news is that AI tools are becoming a great help to these finance professionals with their analytical capabilities and automation.
So, if your organization is also facing pressure due to inefficient workflows and revenue management, then adopting AI cost-saving in healthcare is essential. Click here and let’s get started with your AI-powered journey to delivering better care while reducing costs.
Healthcare organizations can cut costs significantly with AI by automating administrative tasks, speeding up billing and claim processing, optimizing staff scheduling, and reducing diagnostic errors. AI also helps avoid unnecessary tests and hospital readmissions, leading to smarter resource use and better patient outcomes without cutting corners.
To calculate the ROI of healthcare AI, compare the upfront costs (like software, training, and integration) to measurable gains, like reduced admin time, fewer billing errors, improved outcomes, or higher patient throughput. It’s all about whether the savings and efficiencies outweigh the investment over time.
Tasks like prior authorizations, claims processing, eligibility checks, and appointment scheduling offer the highest cost-saving potential through automation. These are repetitive, rule-based, and time-consuming, perfect for AI and RPA to take over, saving staff hours, reducing errors, and speeding up reimbursement cycles.
RCM savings tools help healthcare organizations cut down on billing errors, speed up reimbursements, and reduce manual work. By automating claims, tracking denials, and optimizing revenue cycles, these tools boost cash flow and free up staff to focus more on patient care than paperwork.
CFOs can typically expect to see initial cost reductions from AI-driven initiatives within 3 to 6 months, especially in areas like billing automation or workflow streamlining. However, full ROI often unfolds over 12 to 18 months as systems mature and adoption scales across departments. Patience pays off.
Operations optimization AI reduces clinical care delivery costs by streamlining workflows, cutting down administrative overhead, and improving staff efficiency. It ensures the right resources are used at the right time, minimizing waste, avoiding delays, and letting providers focus more on patient care instead of paperwork.
To track AI-driven cost containment success, focus on metrics like reduced administrative overhead, faster claims processing time, lower denial rates, improved resource utilization, and overall cost per patient. These indicators show if AI is truly helping you do more with less without compromising care quality.
AI-driven budget planning helps healthcare organizations make smarter tech investments by analyzing costs, predicting ROI, and prioritizing needs. Instead of guessing where to spend, leaders get data-backed insights that align tech upgrades with clinical and financial goals, maximizing value without wasting budget.
Finance teams need training in AI budgeting, ROI modeling, and tech fluency to make informed decisions. They should understand how to evaluate AI vendors, spot hidden costs, and align investments with strategic goals because cost-cutting with AI isn’t just about saving; it’s about spending smart.
To ensure sustainable cost reductions with AI, focus on automating repetitive tasks, optimizing resource use, and continuously refining workflows based on real-time insights. It’s not just about cutting costs once; it’s about creating smarter systems that keep improving efficiency over time without compromising care quality.