

Quitting methadone feels like climbing a steep hill that never ends. Many say it's tougher than shaking off heroin because the symptoms drag on. You started methadone as part of medication-assisted treatment, or MAT, to manage opioid addiction. It blocks cravings and eases pain from withdrawal. But now, as you think about stopping, you need to know the real deal on tapering down safely. This guide breaks it all down without judgment. We'll cover symptoms, how long they last, and real ways to handle them. Stick around to learn how to make this journey smoother.
Methadone sticks around in your body longer than most opioids. This sets up a different kind of withdrawal fight. Unlike quick hits from other drugs, methadone builds a slow burn that makes quitting feel endless.
Methadone has a half-life of 24 to 36 hours. That means it takes days for half the dose to leave your system. Heroin clears out in hours, so its withdrawal hits hard but fades fast. With methadone, symptoms start mild but stretch out over weeks. You might feel okay at first, then the real trouble builds. This long action helps in treatment but complicates stopping. Studies show up to 80% of people on long-term methadone face drawn-out withdrawal. It's like a slow leak in a tire—instead of a blowout, you lose air bit by bit.
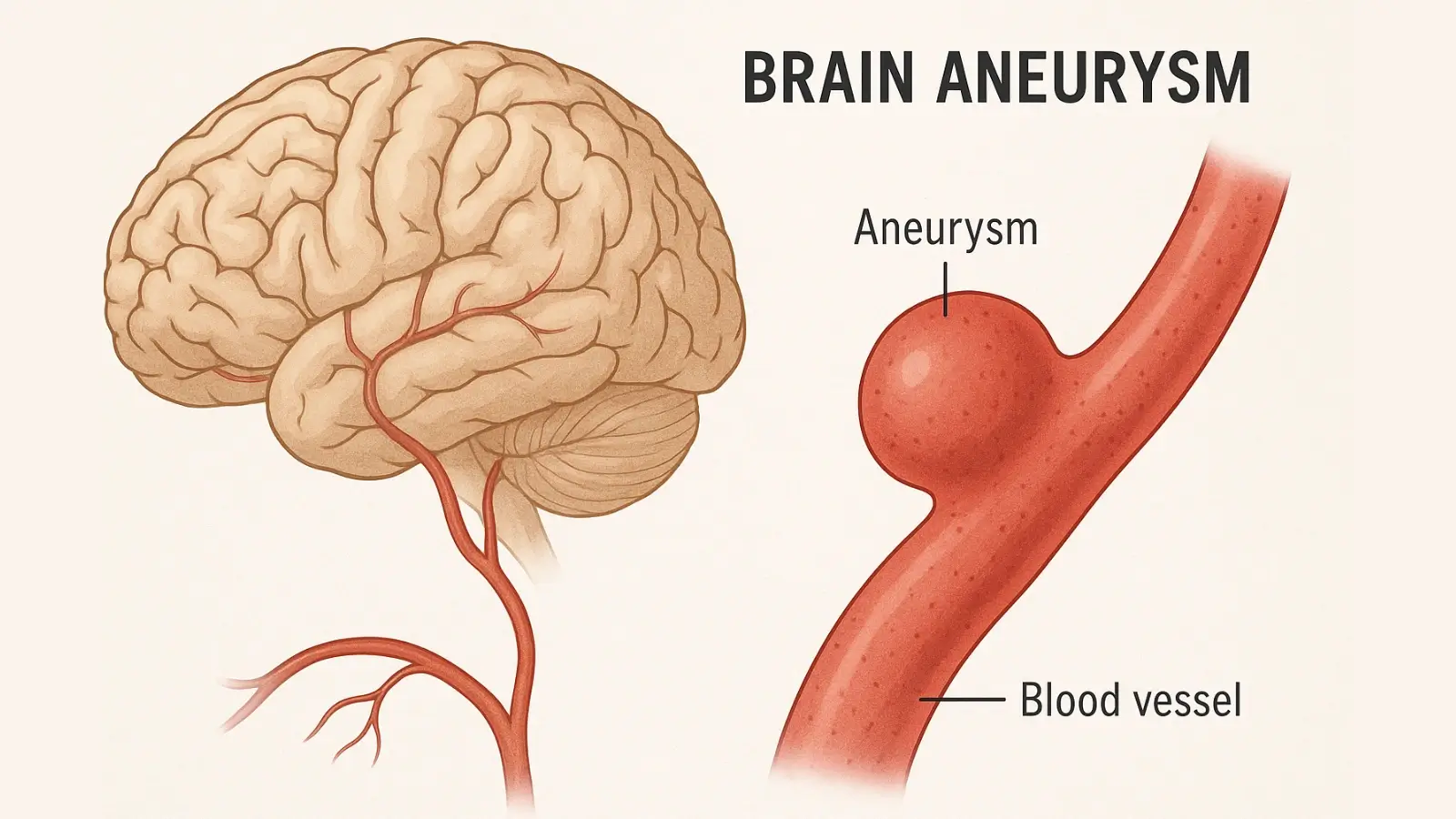
Your body gets used to methadone over time. It downregulates mu-opioid receptors in the brain. These receptors handle pain and pleasure signals. Chronic use means fewer receptors work right. When you cut back, your natural endorphins can't fill the gap. This leads to deep fatigue and mood dips that last. Experts say it can take months for receptors to bounce back. Think of it as your brain's wiring getting rewired after years on the drug. Patience becomes key here, as rushing ignores this biology.
Withdrawal from methadone isn't one big wave. It splits into phases that test you in different ways. Knowing what to expect helps you prepare. Acute symptoms kick in soon after dose cuts. Then come the longer hauls that mess with your daily life.
Right after you lower your dose, your body rebels. Nausea hits like morning sickness on steroids. Muscle aches spread from your legs to your back. Anxiety ramps up, making your heart race. Diarrhea and sweats keep you running to the bathroom. These mirror opioid withdrawal but start softer due to methadone's slow fade. You may yawn a lot or feel chills. One tip: Drink plenty of water with electrolytes. Aim for 8 to 10 glasses a day to fight dehydration. This phase peaks around day 3 to 5 but eases by week two if you taper right.
PAWS is the sneaky part of methadone withdrawal. It lingers for months after the acute stuff fades. Depression settles in like a heavy fog. Insomnia sticks around, leaving you drained. Anhedonia makes fun things feel flat. Anxiety spikes without warning, and energy swings wild—one day you're up, the next you're down. Research from the National Institute on Drug Abuse notes PAWS affects up to 90% of long-term opioid users. Your autonomic system stays off-kilter, causing random hot flashes or gut issues. Set expectations low; this isn't failure, just your body healing slow.
Feelings run hot and cold during methadone detox. Cravings pop up like old habits you can't shake. Mood swings turn small problems into big fights. Leaving the clinic routine feels like losing a safety net. You might question your choices or fear relapse. Many describe it as an emotional rollercoaster without brakes. Why does this happen? Your brain's reward system reboots unevenly. Talk to someone if it gets dark—it's common but doesn't have to define you.
Tapering is your roadmap out of methadone dependence. Skip it, and symptoms explode. Done right, it cuts the pain and boosts success rates. Doctors push for plans tailored to you.
Rapid detox from methadone? Bad idea—it's risky and often fails. Go slow: Drop 1 to 5 mg every one to three weeks. If you're on 100 mg, it might take a year or more to zero out. Addiction specialists customize this based on your dose, health, and history. One study in the Journal of Addiction Medicine found slow tapers raise completion rates by 50%. Always see a pro for your plan. Track symptoms in a journal to spot patterns.
You hit a plateau when symptoms calm at a new dose. Stay there for weeks—let your body catch up. Rushing leads to setbacks. Check stability by noting sleep, appetite, and energy. If things feel steady, plan the next cut. This builds confidence and prevents crashes. Patients often say plateaus feel like small wins on the path.
Shifting from daily clinic pickups to freedom takes work. Space out visits as doses drop—maybe weekly, then monthly. Some switch to buprenorphine if it fits better; it's shorter-acting but easier to stop. Emotional shifts hit hard too—build new routines. Connect with outpatient programs for support. This bridge keeps you accountable without the grind.
Handling methadone withdrawal symptoms needs a full toolkit. Mix meds, habits, and talk therapy for best results. You don't face this alone.
Doctors prescribe non-opioid meds to ease the ride. Clonidine calms high blood pressure and anxiety. It acts on your nervous system without addiction risk. Gabapentin helps nerve pain and improves sleep. For depression, SSRIs like sertraline can steady moods over time. Always get these from a physician—never self-medicate. A caveat: These tools manage symptoms, not cure the process. Combine them wisely under guidance.
Simple changes make a big difference in opioid withdrawal management. Walk 20 minutes daily—it boosts endorphins naturally. Fix sleep with a dark room and no screens before bed. Eat foods rich in B vitamins and magnesium; addiction depletes them. Think bananas, nuts, and greens. Stay hydrated and avoid caffeine spikes. These steps ground you when symptoms swirl.
Therapy pairs perfect with tapering from methadone. Cognitive behavioral therapy, or CBT, rewires negative thoughts. Motivational interviewing keeps you focused on goals. Join 12-step groups like NA or SMART Recovery for shared stories. Hearing others beat PAWS builds hope. Weekly sessions cut relapse risk by 40%, per studies. Lean on these for the emotional lift.
Methadone withdrawal tests your grit, but it's doable with the right steps. Remember, its long half-life means symptoms stretch out—acute hits first, then PAWS lingers for months. Slow tapering is key; aim for tiny cuts every few weeks under doctor care. Manage with meds like clonidine, daily walks, and therapy talks. You've got the tools to handle cravings, moods, and fatigue. Recovery means more than quitting—it's grabbing back your life. Reach out to a specialist today; your fresh start waits.